To say that I didn’t know my great-uncle, Wolfe Levine, would understate things. I didn’t even know of such an uncle, brother of my mother’s father (a grandfather with whom I was close). In retrospect, it’s clear that my great-uncle was simply unmentionable. His story would have been profoundly embarrassing for my grandparents, the first in their immigrant families to join the middle class. We’d write it off now to what we call the stigma of mental illness.
Wolfe Levine’s life story is tragic, dating from an era of large, public mental health institutions that we have sought to put behind us. His journey to the Lima State Hospital for the Criminally Insane in Lima, Ohio, began in 1910 with a criminal conviction: a one-to-five-year sentence in the Ohio State Reformatory in Mansfield for pickpocketing. It was just six years after Wolfe had immigrated to America, at 14. Theft was not a shocking charge against someone who lived in Cleveland with his widowed, single mother and her three other children on a Scovill Avenue block of ramshackle frame houses, along with other Russian Jewish families, near the heart of that community around East 55th Street. Wolfe’s occupations had included “newsboy” and laborer. After his pickpocketing conviction, he would never again be a free man.
Finally, a reason to check your email.
Sign up for our free newsletter today.
State records show that, after less than two years in the state reformatory, Wolfe exhibited “persecutory delusions” and “auditory hallucinations” and was at times “catatonic.” After his struggles at the reformatory—later made famous as the setting for The Shawshank Redemption—he would be sent to the Lima State Hospital, itself the setting for a television film about the Attica prison riot. There, conditions were such that by 1974—some 60 years after Lima State opened—a federal judge chastised the state of Ohio for failing to ensure “dignity, privacy and humane care.” My great-uncle was still there. He would die in state-hospital custody in 1982, at 92, having spent 72 years in institutions. In the language of latter-day reformers, he had been “warehoused” for his entire adult life. His youthful aspiration to be a playwright—the occupation he listed when first admitted to the reformatory—would prove a dark irony for someone formally diagnosed with dementia praecox: schizophrenia, as it later came to be called.
Yet as straightforwardly bleak as it seems, Wolfe Levine’s story is not that simple, especially when one looks more closely at the period in which he lived. His life casts light on how far America has come—and not come—in dealing with the severely mentally ill. And for me, it prompts a question: Given what we know, and the resources that we now possess, are we treating the impoverished mentally ill better today than we did a century ago?
At 20, Wolfe Levine was the eldest of the four children of my widowed great-grandmother, Anna, then 40. Pickpocketing may have been a behavior born of some desperation. His mother could have needed help to pay the rent on the small wood-frame house in which they lived. Wolfe had, in fact, preceded his mother to America, arriving in 1904, two years before she did. He was the immigrant pioneer, mapping the way for his two younger sisters and one brother. At the time of his arrest, his mother was already renting out a room to a boarder, who worked in the house making cigars. (He is listed on the census as a “stogie-maker.”) One daughter, 18, was a baster at a shirtwaist factory; the other, 16, was a packer at a sweater factory. Like his elder brother, Wolfe, my grandfather David, in addition to attending school, worked as a newsboy.
Modern readers will marvel at such a stern sentence handed down for a first offense, but the state reformatory in Mansfield to which Wolfe was sent was aptly named: it was reserved primarily for youthful, nonviolent, first-time offenders. (Others had been convicted of such crimes as abandoning a child, burglary and larceny, and “obtaining property falsely.”) At 20, my great-uncle was still considered young enough to enter such an institution, which appears to have made genuine systemic efforts aimed at behavioral reform, at least if one believes that the proclivity to follow rules and regimens is a positive trait. State records for the Ohio State Reformatory, from June 16, 1910, to June 3, 1911, include the “historical conduct record” for Wolfe and his fellow inmates. At the end of each month, officials filed reports, tracking and characterizing his behavior. These noted how many times he wound up “admonished or reprimanded.” That tally led to “debits or credits,” which, in turn, affected how much of his sentence he would actually serve.
Wolfe did not do well in Mansfield; he saw more than 300 days added to his sentence in just a year’s time. It’s almost certain that this reflected an onset and worsening of his mental illness, for, by April 1912, less than two years after his admission, he was transferred to another state facility. The Columbus State Hospital, a mental institution, was the first way station to his long-term home in Lima. Put another way, his disturbed behavior, perhaps worsened by his internment, led to a decision that he no longer be imprisoned—but not that he be released. Instead, he would find himself treated, by the standards of the day, for mental illness.
The family may have been involved in this decision. My elderly Aunt Rose, my grandmother’s younger sister—now nearly 100 and living in California—recalls her sister and her brother-in-law discussing what to do with Wolfe. “Dave and Ethel were just starting their own family,” she says. “They just couldn’t take care of him.” Not only would they have had a tough time caring for Wolfe; his economic prospects—whether as newsboy or playwright—weren’t promising. Nor was his extended family well-off. My grandmother’s immigrant father was still making deliveries on Cleveland’s East Side with a horse-drawn wagon well into the 1920s. My grandparents, or perhaps Wolfe’s mother, would have had legal grounds to request Wolfe’s commitment. In Mental Illness and American Society: 1875–1940, his definitive history of the public mental hospitals of the era, the late Rutgers historian Gerald Grob explains that the laws of the time “posed no serious obstacle to commitment.” Legal procedures “were administered in a loose and informal manner,” and “commitment was for the most part perceived in human rather than strictly legal terms.”
“The asylums ensured a place for those who could not care for themselves and whose families could not care for them.”
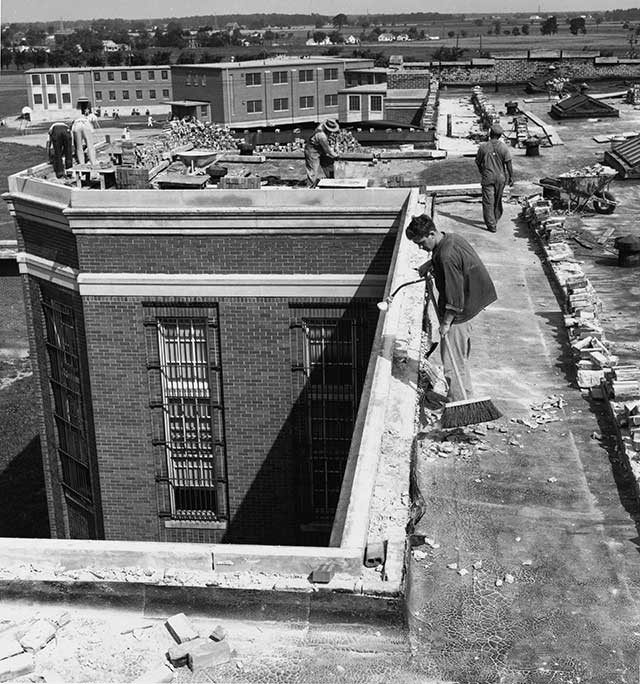
Thus was Wolfe Levine’s road paved to Lima State Hospital for the Criminally Insane, where he arrived in 1915. He was a member of the entering class, as it were, at a facility on which the state of Ohio had invested, over the course of the seven years it took to build, some $2.1 million (about $50 million in today’s dollars). Little information exists on the details of daily life at Lima, but census records portray an institutionalized version of the American melting pot. My great-uncle was listed as a “Russian Jew”; his neighbors—all of whose occupations were listed as “patient”—included many native-born Americans (from Alabama, Indiana, and Ohio), along with others born in Germany, Bohemia, Hungary, England, and Italy. These inmates entered an institution that, like hundreds of others across the country, was enormous in scale: it boasted 17 wings for 1,400 patients and was considered the largest poured-concrete structure in the world prior to the construction of the Pentagon. It provided a safe habitation and a basic level of care for those suffering from what amounted to untreatable severe mental illness. But Lima, especially in the period shortly after it opened, made an effort to do more than simply warehouse its patients.
From Grob’s scholarship, a picture emerges of this time that is more nuanced and, in many ways, more positive than the one commonly portrayed. First, and perhaps foremost, the nationwide system of asylums ensured a place for those who could not care for themselves and whose families could not care for them. As early as the mid-nineteenth century, Grob writes, “virtually every state and territory had at least one mental hospital and many had several in order to ensure equal access for all. That the number of mentally ill patients exceeded available facilities was not an occasion for despair. It was seen rather as an indication of the work that remained to be done.” By 1940, 450,000 patients were institutionalized in public mental hospitals nationwide. The system was the ultimate product of a nineteenth-century reform movement led by Dorothea Dix and Horace Mann, activists outraged by the imprisonment of so many of the mentally ill. Though the care given to the mentally ill was far from perfect, it aspired to be therapeutic—albeit lacking the antipsychotic medications so crucial today in treating schizophrenics, such as my great-uncle, or manic-depressives, who, then and now, constituted the other major group of the severely disturbed. Therapy, writes Grob, included “a balanced diet, a healthful environment, exercise, fresh air, sunlight,” along with various constructive activities, from employment to religious observances to “appropriate amusements.” Many patients, he observes, were better off in the institutions than on the outside, where they lacked care and, often enough, food.
A little-known but remarkable book provides a window into the operations of such hospitals during their heyday. In 1931, 52-year-old Oklahoma journalist Marle Woodson, a former Associated Press foreign correspondent and a Tulsa World reporter, voluntarily checked himself into Eastern Oklahoma Hospital in an attempt to kick his alcohol problem. As he dried out there, he wrote Behind the Door of Delusion, identifying himself as “Inmate Ward 8.” The book offers a generally positive account of the treatment of deeply troubled patients. Woodson developed a respect for the ward attendants, who got to know the inmates well and had a keen sense of when a mild-mannered patient might suddenly turn violent. The attendants themselves were rarely abusive. “There are some brutal attendants in most insane asylums, I have since learned, reliably,” Woodson wrote. “But usually they are weeded out as soon as they are detected in any brutality by the hospital authorities. I have never found but one on this ward.”
Woodson describes not a quiet warehouse but a place bustling with activity. “About me the daytime activities of the hospital hummed,” he observed. “All the work was done by the patients. There was little detailed supervision by the attendants, although they were here, there, and everywhere all the time. One of them would shout an order and the patients, stolidly and mechanically, would carry it out. They seemed to have been trained in the work until it had become almost automatic.” A “floor gang” polished the wood floors, and a crew for making up beds did its work “with a neatness which would shame many of the maids in good hotels.” Others worked in the “art department, bakery, the store, or other departments of the institution.”
There was darkness as well. As Woodson—whose book would be republished by the University Press of Colorado in 1994—writes, “I was to learn that a patient who apparently is in sound mind most of the time can suddenly suffer a paroxysm of wild hallucinations and become thoroughly and irresponsibly insane or even dangerously violent, then, after a period, return to an apparently normal state.” Straitjackets were used on Ward 8 patients; other inmates received opiates or barbiturate sedatives. It’s likely that my great-uncle—so unruly in the reformatory—might have been sedated or restrained. Such were the limited tools then available. Nonetheless, the results were nowhere as grim as the reputation of such institutions today would suggest. Grob references data compiled by a British statistician of nineteenth-century institutions: “Of every hundred cases, 34 percent would recover by the end of one year, 29 percent would die, and 36 percent would remain at the stationary level. A certain proportion of the recovered group would find their way back to an institution after suffering a relapse.”
My great-uncle, of course, was not among those whose condition changed for the better. Nor did he die within a year. In 1950—38 years after entering Ohio’s public mental health system—he was judged “unimproved,” possibly part of the population Grob calls the “chronic but harmless insane.” He then got transferred again, this time to Tiffin State Hospital, a long-term-care facility on the shores of the Sandusky River. In a sense, he had come to have more in common with a larger portion of the population: beginning in the 1920s, public hospitals had doubled as homes for the impoverished senile elderly—another group whose families could not care for them. Such care might be thought of as the hospice care of its time; whatever its shortcomings, it was, at least, available. Wolfe remained at Tiffin until it closed in 1975, and was then transferred back to Lima State. He died there in 1982, and was buried in a Jewish cemetery near Toledo, his burial costs covered by a fund for indigents supported by the Greater Toledo Jewish Federation. He seemingly had been a shell of a human being for decades. Yet he apparently was also kept clean and comfortable over the years, perhaps mentally composing plays that would never be produced.
By the time of Wolfe’s death, the American mental health system that had cared for him for more than 70 years had changed beyond recognition. By the end of World War II and prior to the advent of the policy that would be known as deinstitutionalization, the level of care in facilities like Lima had deteriorated markedly. In a 1946 photo essay headlined MOST U.S. MENTAL HOSPITALS ARE A SHAME AND DISGRACE, Life railed against the “public neglect and legislative penny-pinching” in most states that had allowed “institutions for the care and cure of the mentally sick to degenerate into little more than concentration camps on the Belsen pattern.” Similarly, in 1948, Alfred Deutsch, a journalist and social historian who had previously taken a positive view of public mental hospitals, published an exposé called The Shame of the States. Deutsch was writing not to reject the idea of such hospitals as places for long-term care of the incurably mentally ill but rather to urge renewed public investment in them.
Policy went in a much different direction, however. There is no empirical dispute about the reduction in public support for psychiatric hospitals. Notes the Treatment Advocacy Center, founded by psychiatrist E. Fuller Torrey: “The United States is in the midst of a psychiatric bed shortage that worsens every year. By early 2016, the practice of closing state mental hospitals, often called ‘deinstitutionalization,’ had eliminated more than 96% of the last-resort beds that existed in the mid-1950s; after a brief period of expansion in the 1990s, private hospitals, too, are shrinking their psychiatric inpatient capacity.” In 1955, Torrey points out, 560,000 patients resided in state psychiatric facilities; by 2015, the number had fallen to 45,000. This dramatic change was not the result of a decreased need for these facilities but of an intellectual movement against such care for being repressive. Deinstitutionalization advocates saw asylums, in Grob’s words, either as manifesting “a generalized fear of social disorder” or as the result of “the rise of market capitalism and its concomitant demand for greater productivity.” Hospitals existed to warehouse “social deviants” or “unproductive persons.”
These days, as a consequence of deinstitutionalization, many of those suffering from severe mental illness—schizophrenia or manic-depressive disorder, as well as clinical depression—are housed in prisons and jails. The Bureau of Justice Statistics has estimated that 365,000 adults with serious mental illnesses are behind bars, and an additional 770,000 are on probation or parole. Chicago’s Cook County Jail has been described as the nation’s largest mental hospital; the Treatment Advocacy Center has reported that ten times as many seriously mentally ill persons are behind bars than in state hospitals. A Department of Justice study estimates that half of all inmates have a mental illness or substance-abuse disorder and that 15 percent of state prison inmates are diagnosed with a psychotic disorder.
Those who develop severe mental illness once incarcerated may be treated with medications that did not exist in my great-uncle’s time. The Bureau of Prisons estimates that, between 2010 and 2014, some $36.5 million was spent on psychotropic drugs in the federal prison system alone. It estimates that 10 percent of the 216,000 inmates received medications designed to treat conditions ranging from depression and bipolar disorder to acute schizophrenia. There’s no guarantee that those suffering from mental illness will receive treatment, though. In a November 2016 class action in Alabama, attorneys representing inmates asserted that the “prison system fails to identify mental illness in many inmates and understates the severity of illness in others.” In a January 2015 paper in the Journal of the American Medical Association, Dominic Sisti, Andrea Segal, and Ezekiel Emanuel, all of the University of Pennsylvania’s Perelman School of Medicine, write that “it is difficult to imagine how ethically sound treatment of mentally ill prisoners can be delivered. It may be impossible for prison psychiatrists—who may have dual loyalties to the patient and the institution—to provide inmates with compassionate, private and patient-centered care.”
“A key problem: the risk of disruption or the prospect of suicide leads authorities to isolate mentally ill inmates.”
A key problem: the risk of disruption or the prospect of suicide leads authorities to isolate mentally ill inmates; the only other alternative is to let these individuals circulate in the general prison population. Such an unpalatable choice reflects the fact that a system of hospitals for the “criminally insane”—that is, those judged guilty of crimes and exhibiting signs of mental illness while in prison—is no longer available. For mentally ill inmates, Sisti, Segal, and Emanuel believe, the current system is a long way from an “asylum—a protected place where safety, sanctuary, and long-term care for the mentally ill would be provided.”
Nor does anything preclude inmates with severe mental illness from being released once they’ve completed their sentences—with no guarantee of their receiving what’s known as assisted outpatient treatment once they’re no longer behind bars. Imagine a latter-day Wolfe Levine, suffering from delusions, returning to his poor, immigrant neighborhood, either to await arrest for another infraction or to complicate life for his family. Such people frequently wind up on the streets now. The Department of Housing and Urban Development estimates that, of some 564,000 homeless individuals identified on a single day in January 2015, some 25 percent—140,000—were seriously mentally ill; 31 percent were classified as unsheltered, meaning that they live on the street, in abandoned buildings, in cars, or in the sort of large encampments found in some cities, including Portland and Seattle. Those familiar with this population say that it is common for the mentally ill homeless to commit new crimes—and to return to prison, where they’re at least sheltered and likely to get their needed medication.
Their families often find themselves unable to cope with the problems that may ensue. A person who threatens violence, but as yet has committed no crime, may not be involuntarily committed to any of the small number of public mental hospital beds that remain. No one can force the seriously mentally ill to take their medication. Families may call police if a mentally ill family member threatens violence—often leading to confrontations that don’t end well.
Of course, it’s possible today that someone like my great-uncle could receive medication in prison, respond positively, and, on his release, continue to have access to medical help, maybe even going on to lead a relatively healthy life. Yet it is equally likely that such a young man would be put in isolation for the remainder of his term of confinement and, upon release, shortly cause harm to someone in the outside world. In his 2013 book American Psychosis: How the Federal Government Destroyed the Mental Health System, Torrey, citing National Institute of Mental Health data, estimates that 1 percent of the 12.3 million people estimated to suffer from serious mental illness are a threat to themselves or others. That amounts to 123,000 such persons—including those who push subway riders onto the tracks or open fire at college campuses.
It is in this context that we should regard again the institutions of the earlier era. Wolfe Levine may have been “warehoused,” in the common term—but he harmed no one, notwithstanding what were almost certainly schizophrenic delusions. He may have found satisfaction in helping with the chores at the hospital; he may have been comforted by visits from a Toledo rabbi; and he was, without doubt, safe and warm throughout the cold Ohio winters.

Yet is it practical to try to restore the lost options provided by the once-sprawling state mental hospital system? Providing for the most severely mentally ill does not imply that a hospital system of such a scale should be re-created. At their height, such hospitals, their names notwithstanding, housed many besides those suffering from mental illness—including the indigent, the senile elderly, and others suffering from what were then incurable, debilitating diseases, such as syphilis. The population that would have to be addressed today—those 123,000 whom Torrey identifies—is not unmanageably large. As Sisti, Segal, and Emanuel put it: “Reforms that ignore the importance of expanding [asylums] will fail mental health patients who cannot live alone, cannot care for themselves, or are a danger to themselves and others.” Institutions could also be the sites for short-term, assisted outpatient treatment.
It’s worth rediscovering the sentiment expressed by Adolph Meyer, a physician on the staff of the Kankakee (Illinois) state asylum, in 1893. Meyer believed that the state had an obligation to provide every insane person with “the benefit of treatment and supervision by a competent physician.” We might argue about whether those who can afford such treatment on their own, or whose families can afford to help them, should receive public assistance. But leaving Wolfe Levine’s successors on the street or in isolation behind bars suggests that—in practice, at least—we have become not more but less compassionate about the severely mentally ill.
Top Photo: Wolfe Levine was first confined at age 19 and would spend the rest of his life in institutions, . . . (OHIO HISTORY CONNECTION)

