The story of Gregory Seifert represents everything wrong with New York’s mental health system. Last year, while touring the Erie County Holding Center—better known as the Buffalo Jail—I observed him quietly hallucinating in his cell, probably communicating with his superiors at the CIA, where he claimed to work. Police had arrested him 14 months earlier for cutting down three wooden power poles with a chainsaw, terminating power to 6,800 homes in suburban Buffalo in the dead of winter. Like most individuals with chronic paranoid schizophrenia, he doubtless had a logical (in his mind) reason for his actions: perhaps his voices told him that cutting off power would prevent a tsunami from Lake Erie from sweeping over Buffalo. When the police questioned him, though, Seifert denied everything. “I know this sounds weird,” he said, “but my cloned twin did it.”
Seifert hadn’t always heard voices. He had graduated from college with a degree in finance, got married, had four children, and held down a good job. But during his thirties, he suffered the onset of paranoid schizophrenia, and, worse, he had no awareness of his illness—a condition called anosognosia, which results from the disease’s effects on the parts of the brain we use to think about ourselves. From there, it was all downhill. As described vividly by Matthew Spina in the Buffalo News, Seifert lost his job and family, became homeless, set fire to his car (he thought it contained devices to spy on him), and was psychiatrically hospitalized for brief periods in community hospitals seven times, including just two weeks before chainsawing the poles. He mostly refused medication. After all, he thought he was fine.
Finally, a reason to check your email.
Sign up for our free newsletter today.
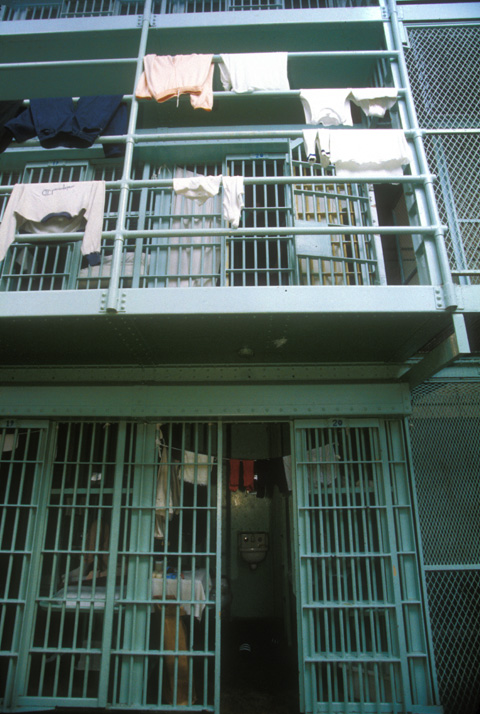
Seifert’s stay in the Buffalo Jail was a difficult experience for him and everyone else there. Because of his illness, he broke jail rules, trashed his cell, and set fire to pillow stuffing that he had jammed into an air vent, which brought additional felony charges of second-degree arson. Yet he would not have been in jail at all if his schizophrenia had received appropriate treatment. Tragically, his family’s efforts to get him medical help ran up against New York’s laws, which make the involuntary commitment of adults exceedingly difficult. And even if the laws encouraged commitment, finding a place to treat him would have been hard, too. These days, the Buffalo Psychiatric Center, a state hospital originally built to care for more than 3,500 people like Seifert, only has 190 beds, and they’re invariably full. Buffalo Psychiatric is architecturally a National Historic Landmark, its sandstone Gothic towers once standing as a symbol of the state’s enlightened protection of the sickest patients; they’re now a symbol of the state’s terrible neglect of such patients. Over the last several decades, New York State has downsized not just the Buffalo center but all of its state mental hospitals, which went from having 96,664 beds in 1955 to just 3,300 today—and the number keeps dropping. When the mentally ill do manage to get care, it’s often in the psychiatric units of community hospitals, where federal Medicaid and Medicare cover most of the costs, saving the state money—an incentive to further reductions. Claims that the seriously mentally ill get better care in community hospitals are nonsensical. Most such hospitals aren’t set up to look after the most difficult patients and tend to discharge them as quickly as they can.
The state’s abandonment of Seifert and similarly sick individuals leads to immeasurable human tragedies and very measurable social costs. Once a leader in public psychiatric services, New York State now shows how not to treat the mentally ill.
Make no mistake: there are many Seiferts in New York’s jails and prisons. A study done between 2002 and 2006, covering inmates in three New York county jails, reported that 15 percent of the males and 31 percent of the females suffered from a current serious mental illness, narrowly defined to include schizophrenia, bipolar disorder, and major depressive disorder. These percentages are almost certainly low, moreover, since 31 percent of the inmates refused to participate in the study, and their ranks would have included many mentally ill people, especially those with paranoid schizophrenia, who’d be suspicious of such surveys. Since then, most agree, the number of mentally ill in jails has only increased. It thus seems reasonable to estimate that about 20 percent of jail inmates now have a serious mental illness, though this total would vary from jail to jail. In October 2013, the New York State Commission of Correction counted 29,235 inmates in state jails, including 11,903 in the vast Rikers Island complex in New York City. That would mean that approximately 5,800 mentally ill people are currently incarcerated in New York jails. As for the prisons, the U.S. Department of Justice estimated in 2005 that 15 percent of the nation’s state prisoners “met the criteria for a psychotic disorder,” meaning that the inmates experienced delusions, such as “a belief that other people were controlling their brain,” or hallucinations. This finding is consistent with more recent data. As of late 2013, New York had 54,531 state prisoners, so we can safely assume that at least 8,200 of them suffered from a serious mental illness. That adds up to a minimum of 14,000 inmates with serious mental illness (not counting substance abuse) in New York.
These figures represent a big step backward in how we deal with mental illness. Even by the 1830s, Americans increasingly considered it inhumane to lock up mentally ill individuals in jails and poorhouses, which had long been the common practice. A broad social movement of that era, led by activist Dorothea Dix, among others, succeeded in building the first state psychiatric hospitals and in getting mentally ill prisoners transferred en masse to the new institutions. When Worcester State Hospital opened in Massachusetts in 1833, more than half of the first-year admissions arrived from jails, prisons, and poorhouses. The movement of the mentally ill into mental hospitals proceeded over the next several decades, so that by 1880, a national census of mentally ill individuals—still the most complete such survey done in the United States—found that less than 1 percent of jail and prison inmates were “insane persons.” That the mentally ill deserved treatment, not jail cells, continued to be the prevailing view for most of the next century. Studies of prisoners regularly reported low rates—usually 3 percent or less—of serious mental illness among them.
Then, during the 1960s, effective medications for treating mental illness became available, and the deinstitutionalization of state mental patients got under way. Deinstitutionalization’s fundamental flaw was not its shifting of patients from hospitals to living in the community but its failure to ensure that those patients would keep taking the medication they needed to remain well once they left the hospital.
For that, one can blame, at least in part, the lawyers. In 1970, the New York Civil Liberties Union (NYCLU), under the direction of lawyer and human rights activist Aryeh Neier, began the Mental Health Law Project. Its purpose was to empty the mental hospitals. Neier and his allies won a series of lawsuits, changing the laws in most states, including New York, to make involuntary hospitalizations virtually impossible unless the mentally ill were an “imminent danger” to themselves. Bruce Ennis, the lead lawyer on several of the project’s court cases, was frank in stating the aim: “nothing less than the abolition of involuntary hospitalization.”
The tragedy that ensued was captured by infamous cases like that of “Billie Boggs” (real name: Joyce Brown), a mentally ill homeless woman living on East 65th Street in New York during the 1980s. Despite Brown’s urinating in the gutter, defecating on the sidewalk and on herself, tearing up money given to her by passersby, running unpredictably into traffic, and wearing little clothing even in cold weather, the NYCLU successfully blocked multiple attempts by the city to have her psychiatrically hospitalized. Since individuals like Brown could no longer be forced to receive care as a condition of remaining free, many wound up getting charged with misdemeanor crimes and sent to jail. Even Neier would acknowledge the ruinous consequences. In his 2003 memoir, Taking Liberties, he wrote: “Unhappily, I concede that deinstitutionalization of the mentally ill was a civil liberties success but, for many of those released and for their urban neighbors, a social policy failure.”
Already by 1972, Marc Abramson, a young psychiatrist in San Mateo County, California, had noted a rapid increase in mentally ill inmates in the county jail and published an article describing “the criminalization of mentally disordered behavior.” He also quoted a California prison psychiatrist claiming to be “drowning in patients.” Prophetically, Abramson wrote that “those who castigate institutional psychiatry for its present and past deficiencies may be quite ignorant of what occurs when mentally disordered patients are forced into the criminal justice system.” Today, this shift is virtually complete: we have regressed to where we were in the 1830s.
One can see this sad history reflected in the very buildings and grounds of New York’s prison system. Gowanda State Hospital, south of Buffalo, opened in 1894 and eventually housed more than 4,000 of the seriously mentally ill; nearly 100 years later, the state closed the hospital and turned it over to the Department of Corrections, which now operates two state prisons on the premises, together holding 2,535 medium- and maximum-security male felons. Assuming that 15 percent, or 380, of these men have a serious mental illness, it’s entirely possible that some could have been treated in the state hospital as young men, been discharged without adequate follow-up treatment, committed a crime related to their untreated mental illness, and now occupy prison cells on the same grounds. They might even be in the same building, since one of the prisons uses one of the old state hospital structures. Another example: Willard State Hospital, on the shore of Seneca Lake, opened in 1869 for 1,500 patients—the largest state hospital in the nation at the time, said to provide “for the dependent insane with a maximum of humanity, efficiency and economy.” It closed in 1995. The Department of Corrections currently uses its buildings as a treatment facility for 916 state prisoners suffering from drug addiction.
The site of the Central New York Psychiatric Center may be the most striking example of this institutional shift. The grounds were originally home to Marcy State Hospital, a mental hospital opened in 1919 that eventually came to house more than 3,000 patients. My sister, who had schizophrenia, was hospitalized there for almost 25 years. In 1981, the state government closed the hospital and turned over the site—you guessed it—to the Department of Corrections, which used it for two state prisons, Marcy Correctional Facility and Mid-State Correctional Facility, together holding 2,558 maximum- and medium-security prisoners. In recent years, as the number of mentally ill individuals in these and other state prisons swelled, someone in Albany got the idea of grouping the most seriously ill patients in one location. So they constructed a third building on the site and called it the Central New York Psychiatric Center—a 226-bed, maximum-security prison hospital for the most mentally ill prisoners. (It also accepts some mentally ill transfers from upstate jails.) Most of the new hospital’s inmates come there, of course, after getting released from state psychiatric hospitals with inadequate follow-up treatment and then committing a crime, in the all-too-familiar pattern. When the Central New York Psychiatric Center opened in 2009, Governor David Paterson proudly called it a “cutting-edge program” that “represents government at its best.” Jonathan Swift would surely have had something to say about that.
Putting people like Gregory Seifert in New York’s jails and prisons causes many problems for institutions and inmates alike. In the Rikers Island Jail, the average inmate stay is 42 days, but for those with a serious mental illness, it is 215 days. The mentally ill are less likely to make bail and more likely to break jail rules, thus failing to get their sentences reduced for good behavior. They also usually cost more to incarcerate on a daily basis than other prisoners, especially if one includes the price of medications. In Florida’s Broward County Jail, the difference is $130 per day versus $80 per day; in the Texas prison system, the difference is $40,000 per year versus $22,000 per year. Mentally ill prisoners are three times more likely to be raped or otherwise victimized by other prisoners. As noted by Spina, who has written passionately about this injustice, a mentally ill individual in prison “is like a lamb or a zebra to a lion—easy pickings.” Psychotically induced behavior can also be extremely disruptive to daily life behind bars. A loudly hallucinating prisoner can disturb an entire prison or jail unit. As a deputy in a Mississippi jail put it: “They howl all night. If you’re not used to it, you end up crazy yourself.” Such behavior often results in solitary confinement for mentally ill prisoners, which usually produces a further deterioration of their psychiatric condition. Studies in some states have reported that half or more of the prisoners in solitary confinement are mentally ill.
Keeping inmates from killing themselves is a major worry for jail and prison officials, and suicide attempts occur, as one might expect, disproportionately among mentally ill prisoners. In the King County, Washington, jail system, a 2002 study found that three-quarters of inmates who attempted suicide had “a chronic psychiatric problem.” In California’s prison system, three-quarters of inmate suicides “had a history of mental health treatment,” another study from the 2000s found. The problem was vividly on display during my visit to the Erie County Holding Center, which had separate units for close observation of any prisoners suspected of being suicidal. In one, I observed a guard sitting behind a glass wall, closely watching three inmates wearing paper gowns in a large, well-lighted cell. The guard could see the prisoners everywhere, including in the bathroom, and someone had to be on watch around the clock.
I discussed the suicide issue with Timothy Howard, the elected sheriff of Erie County and director of the Erie County Holding Center. He and his staff aren’t just responsible for the 680 inmates in the Holding Center but also for 1,070 more in the annex in nearby Alden. Sheriff Howard has held the office since 2005 and is proud of his position—in 1871, he reminds me, Grover Cleveland was elected sheriff of Erie County and, from there, went on to become mayor of Buffalo, governor of New York, and finally president of the United States. Howard will be the first to say, though, that jails shouldn’t be used as mental hospitals. He can provide psychiatric medications to inmates who agree to take them, but for individuals like Seifert, who don’t understand that they’re sick, he has few options. New York State regulations do allow him to transfer, at the jail’s expense, such inmates to the Department of Corrections psychiatric hospital at Marcy, but the beds are almost always full there. Howard thus winds up with acutely and chronically psychotic inmates whom he cannot treat, yet for whom he’s held responsible if they hurt themselves or others. It’s an impossible job.
So what should we do instead? New York once was a model for its provision of mental health services. In 1954, it became the first state to pass community mental health legislation. The next year, it was one of the first two states to make chlorpromazine, a new antipsychotic, available in state hospitals. During the postwar years, the New York State Office of Mental Health was led by professionals regarded as exemplars of their field. For New York, or any state, to show such leadership again, five things will need to happen.
First, the state will need to have a sufficient number of public psychiatric beds. A 2008 report from the Treatment Advocacy Center, a nonprofit organization I founded, recommended approximately 50 public psychiatric beds per 100,000 population as the minimum needed. Based on New York’s population, this adds up to approximately 9,750 public psychiatric beds needed in the state—almost three times the 3,300 currently available. Nobody is recommending a return to the 1950s, when New York had almost 97,000 beds, but their reduction has clearly gone way too far.
Second, the state will need to pass an inpatient commitment law that allows for the forced hospitalization of seriously mentally ill individuals in need of care—before they end up in jail or prison. New York’s current inpatient statute is among the strictest in the nation in its criteria for involuntary hospitalization.
Third, New York already has a great tool for mental health leadership—an assisted outpatient treatment (AOT) law—but officials must be willing to use it. This kind of treatment, instituted by court order, with periodic judicial review, basically says to a seriously mentally ill person like Seifert: we know that you’re mentally ill and not aware of your illness; and we know that when you do not take your medication, you become a danger to yourself and to others. Therefore, we require that you take your medication as a condition for living in the community. If you don’t, you return to the hospital. Studies of AOT measures have shown them to be highly effective in reducing rehospitalization and incarceration. New York’s AOT law, named after Kendra Webdale, who was pushed to her death under a subway by a man with untreated schizophrenia, is being well used in New York City and in a few other counties, such as Greene, Rensselaer, and Columbia. Unfortunately, some counties, including Erie County, Seifert’s home, rarely use it. Here, one can blame lack of leadership in the state’s Office of Mental Health, especially under Commissioner Michael Hogan from 2007 to 2012. The recent appointment of Dr. Ann Marie Sullivan to this post is widely regarded as more promising. Part of Seifert’s tragedy is that, with his history of medication noncompliance and past behavior, he was an ideal candidate for AOT. If Seifert had lived in Troy, in Rensselaer County, instead of in Buffalo, in Erie County, he would probably have been placed on AOT and never chainsawed those power poles. For a mentally ill person in New York State, what county you live in can determine your fate.
Fourth, a state must have an effective way to treat the seriously mentally ill who do wind up in jail or prison. New York, compared with other states, does poorly in this area. For example, New York does not authorize the use of involuntary antipsychotic medication in prisons. Most states approve such measures, which the U.S. Supreme Court approved in 1990 in Washington v. Harper. To medicate Seifert involuntarily while in custody, the Erie County Holding Center would have had to transfer him, if a bed could be found, to a state mental hospital or to the prison hospital at Marcy.
Finally, politicians will need to show vision. This is particularly vital because the mentally ill, lacking a strong lobby, usually get lost in the political process. Sadly, New York State has had no political leaders willing to speak for the mentally ill in recent years. Governor Andrew Cuomo has shown zero interest in this issue—indeed, he has proposed to close six more state psychiatric hospitals.
Gregory Seifert spent more than a year in the Erie County Holding Center, during which his mental illness went untreated. A judge at last ordered that he be sent to the Rochester Psychiatric Center, where he received appropriate treatment, his schizophrenia went into remission, and he was discharged to the community. In a better system, he never would have been sent to jail.
The transfer of mentally ill individuals from mental hospitals to jails and prisons has been a policy disaster. Sheriff Tom Dart, who runs Chicago’s Cook County Jail, puts it bluntly: “I can’t conceive of anything more ridiculously stupid than to do what we are doing right now.” Many mentally ill people have thinking disorders. But could their disorder be any worse than the one exhibited by New York State officials carrying out the present policy?
Top Photo: THE GRANGER COLLECTION, NYC

