In 2017, feeling thwarted and bilious after almost two decades as a lawyer, I began taking classes at a Manhattan psychoanalytic institute, with the goal of changing professions. Among my classmates, along with the expected physicians, psychologists, and social workers, were humanities Ph.D.s, journalists, and a college administrator. After looking at the world through a single window for so long, I was happy to engage with new perspectives. In some ways, law and psychoanalysis hold similar attractions, including guild membership and the promise of recondite knowledge. Both professions are seductive to those whose idea of themselves is bound up with their intellect. Legal reasoning, though, tends to take logic as its ideal and its limit. What analysis offered was a return to the mystery of human personality.
After several decades of declining influence, psychoanalysis is now enjoying a revival of public interest and intellectual esteem. Recent graduates from the analytic institutes are finding their services in demand. Gone is the dour, conventional, Germanic Sigmund Freud we knew when psychoanalysis was the dominant mode in postwar American psychiatry. That Freud was an anti-utopian, who once joked that the goal of analysis was to replace neurotic misery with ordinary human unhappiness. Now we have the anarchic Freud, the sexual liberator, the enemy of repression. This battle over the true meaning of his work began when he was still alive and has never really stopped. Freud now seems to have been repurposed for a new era of consumer demand.
Finally, a reason to check your email.
Sign up for our free newsletter today.
Psychoanalysis’s golden age in America began at the end of World War II, with the return from Europe, Asia, and North Africa of traumatized veterans needing psychiatric help. Successfully lobbied by the pioneering American analyst Karl Menninger, among others, the Veterans Administration started funding psychoanalytic approaches to treating these men. Partly as a result, analysis, previously in vogue mainly in avant-garde artistic circles, grew rapidly as a profession.
By the early 1960s, most American psychiatrists working outside of institutional settings were analytically trained. Privileged and austere, they formed a secular priesthood. Analysis was regarded not just as an advance in the treatment of mental illness but, more romantically, as part of a larger humanistic project. The influence of analytic ideas in the humanities was considerable, with psychoanalytic literary and film criticism enjoying vogues. The core Freudian notion that human beings are inherently irrational actors even influenced early versions of behavioral economics. To be conversant in analytic terminology symbolized one’s belonging to an intellectual elite.
Analysis is founded on a few deceptively simple concepts: the claim that early childhood experience is decisive in the formation of personality; the idea that, far from the disciplined and purposive actors we believe ourselves to be, we are motivated by unconscious desires; the centrality of sexuality, especially those desires we repress; and the notion that the stories we tell ourselves, especially about our own past, are false or incomplete. Those stories make up both the foundation of our identity—the “I” of Western society consists of such experiences and affinities—and potentially the bars to our cages, because they trap us in patterns of thought and feeling that may lead us to destruction. The patient comes to treatment because he is suffering, yes—but more fundamentally, because he has reached a narrative cul de sac.
As British analyst Adam Phillips observes, “The aim of treatment [is] the modification of symptoms and the alleviation of suffering through redescription.” The core “technology” of psychoanalysis is free association, in which the patient verbalizes whatever thoughts come to his mind, with as little self-censorship as possible. The analyst then sifts through these thoughts, not to understand what the patient intends to express, but what he has expressed unconsciously—that is, what has become so much a part of his narrative that he takes it for granted. “I have missed my opportunities” or “My relationships always end badly”—such unexamined beliefs shape our behavior and become self-fulfilling prophecies. The analyst draws the patient’s attention to this latent content, hoping that it might be reshaped into a story that gives the patient more agency and self-respect. The patient does not cease to suffer—suffering, for Freud, is the price of civilization—but might begin to find his misery more bearable. In turn, when we believe in our ability to bear life’s suffering, we can begin to live more fully.
Many early patients testified to the transformative effect of analytic treatments. As the dominance of psychoanalysis grew, however, the theoretical absurdities piled up. Freudians bizarrely maintained, for example, that autism in children resulted from maternal coldness. For decades, analysts regarded homosexuality as a mental disorder, the product of abnormal psychosexual development. Analysts also contributed significantly to the recovered-memory scandals of the 1980s and 1990s, igniting a panic that led to false accusations of child sexual abuse, destroying families and causing the wrongful imprisonment of parents and day-care workers. Psychoanalysis came to be identified with an adamantine, self-righteous, and irresponsible intellectual style.
From its beginnings, analysis was plagued by doubts about its effectiveness. But analysts who believed that they were having extraordinary experiences in their treatment rooms were reluctant to subject their beliefs to investigation. After all, they were engaged in the refashioning of human personality—what relevance could the randomized clinical trial have to such an enterprise? Even friendly critiques were dismissed as “resistance” to the painful truths that analysis was exposing. And because analysis was expensive and its patients frequently drawn from the wealthy and intellectually adventurous, it came to be seen as elitist and remote from the problems of ordinary people. Rather than engage these criticisms, the analytic establishment pulled up its drawbridges.
The dominance of psychoanalysis ended just 35 years after it began, with the publication, in 1980, of the third edition of the Diagnostic and Statistical Manual (“DSM-III”)—the standard psychiatric desk reference—which essentially wrote psychoanalysis out of the American psychological mainstream. By then, biological approaches to the study of mental disorders were getting most federal research funding and were thought likelier to provide fresh insights.
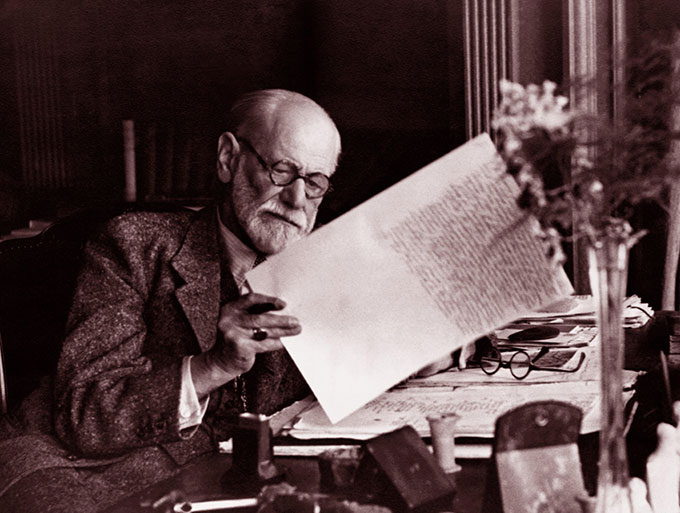
Psychoanalysis began with Freud but doesn’t end with him. Indeed, the field has periodically been riven by personal rivalry and doctrinal differences, including the question of whether nonphysicians should be trained as analysts, which was not decided in the United States until 1988, with the settlement of an antitrust suit brought by psychologists. (The exception was New York psychoanalytic institutes, which had been training “lay analysts” for decades.) Freud always supported the training of nonphysicians as analysts. “Psychoanalysis,” he wrote in The Question of Lay Analysis (1926), “is a profession of lay curers of souls who need not be doctors and should not be priests.” The training in large numbers of psychologists, social workers, and others buttressed analysis at a time when medical students training in psychiatry had begun to prefer other methods. It also deepened the epistemological divide between those who saw mental illness as a biological phenomenon and those who favored approaches founded in the humanities.
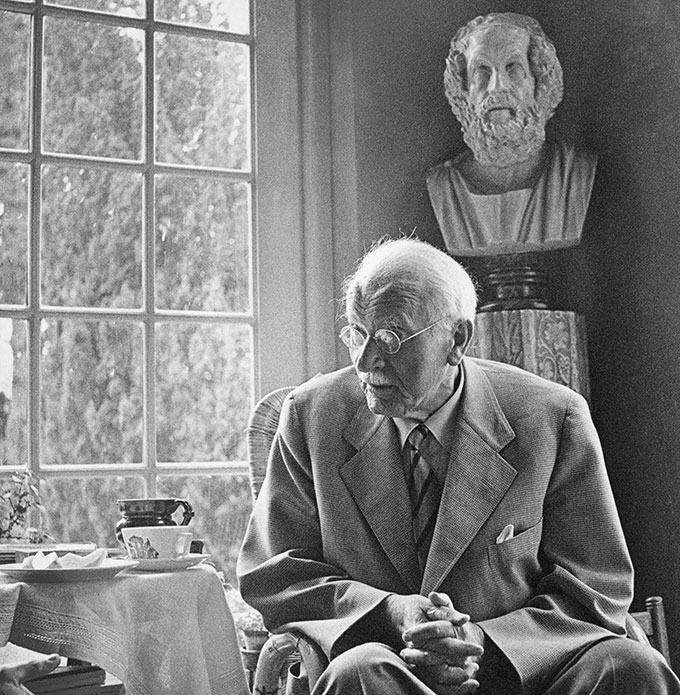
A former Freud disciple, then an apostate, Carl Jung went on to become almost as influential as Freud himself. (Jung is associated with the idea of the collective unconscious, which holds that human beings are connected with one another and with their forebears through a set of shared experiences, which result in behavioral patterns that we recognize as “archetypes.” Canadian psychologist Jordan Peterson is a noted Jungian.) In the 1950s and 1960s, Melanie Klein, Donald Winnicott, and Bruno Bettelheim influenced the development of the field and became intellectual stars beyond it. Analysts today are divided into many subgroups, each with its own way of understanding neurosis and treatment-room dynamics. Freud’s writings nonetheless remain the common source for most strains of psychoanalytic thought, and Freud’s personal celebrity remains one of the field’s core assets.
Despite the declining prestige of psychoanalysis, we still argue about Freud, partly because nothing very satisfying has come along to replace him. Andrew Scull writes in his engrossing history of American psychiatry, Desperate Remedies: Psychiatry’s Turbulent Quest to Cure Mental Illness (2022): “[T]wo centuries after the psychiatric profession first struggled to be born, the roots of most serious forms of mental disorder remain as enigmatic as ever. . . . [T]he diagnostic manuals psychiatrists have created and relied on have become increasingly unwieldy, and the consensus about the categorization of mental illness has threatened to fall apart.”
We have not replaced benighted Freud with rational “science” because that science—which today means, among other things, the use of MRIs to study brain function in people with schizophrenia, bipolar illness, and other disorders—offers such artless explanations. (“The patient is ill because she has deficits in several neurocognitive domains” merely restates the problem.) In some ways, our understanding of mental illness remains medieval, our ideas as ill-formed as humorism and trephining. Billions of dollars of brain research have yielded—what, exactly? We await the transformative discovery, something akin to the germ theory of disease, that will set research and treatment of mental disorders on a more productive course.
If psychoanalysis is the God that failed, then SSRIs and cognitive behavioral therapy (“CBT”) are the magic bullets that didn’t fire. The introduction of Prozac in 1987 for the treatment of major depressive disorder was met with tremendous optimism. The drug initially seemed like a breakthrough treatment for a disease with a lifetime incidence rate of more than 10 percent of the U.S. population. Peter Kramer’s galvanic 1993 book, Listening to Prozac, played an enormous role in popularizing this class of drugs, despite the author’s misgivings about their widespread adoption. Kramer, who is analytically trained and later wrote a sympathetic biography of Freud, found that after taking the drug, some of his chronically depressed patients became suddenly less inhibited, more joyous—in his coinage, “better than well.”
The use of SSRIs is founded on the “serotonin hypothesis,” the claim that reduced levels of serotonin in the brain are the biological cause of depression. More than three decades after Prozac won FDA approval, however, the link between serotonin and mood remains conjecture. Of course, it might be that SSRIs are effective for some reason that we don’t yet understand, in which case making them a first-line treatment would still be appropriate. (The point is that the patient resumes flourishing, not that we have an elegant explanation.) As reflected in many controlled trials, unfortunately, the efficacy of SSRIs has proved disappointing, only slightly better than a placebo. It would be tendentious to claim that they help no one. They are not, however, a solution for major depressive disorder, and they have significant side effects.
Cognitive behavioral therapy, with theoretical roots in psychoanalysis and philosophical roots in ancient Stoicism, has replaced analysis as the dominant form of talk therapy in the United States. CBT originated as a form of treatment for depression, but its use has expanded to treat substance abuse, marital conflict, posttraumatic stress disorder, anxiety, and eating disorders. CBT seeks to reduce a patient’s undesirable symptoms by attacking the cognitive distortions that lead to emotional dysregulation. The CBT practitioner listens, seeking to identify errors in the patient’s thinking. He gives due weight to the patient’s experiences but is more focused on symptoms than on personal history. His goal is simply to return the patient to normal functioning.
Initial CBT trial results were encouraging, which led to its rapid promotion as the “evidence-based” “gold standard.” (Insurance companies like CBT because it promises rapid symptom relief, making it less expensive than more open-ended forms of therapy.) Subsequent trials have shown smaller effects than was initially hoped, however, with only about half of anxiety sufferers, for example, exhibiting a clinically significant response. Study results also suggest that CBT is not very effective at treating schizophrenia or bipolar disorder or major depression.
Critics argue that CBT cannot be the standard therapy because it is based on an impoverished view of the causes of mental illness. Suffering is not a “problem” to be solved like a sinus infection. It is a philosophical conundrum, bound up with our very existence. Learning to tolerate suffering, and even make meaning from it, is the project of a lifetime.
My fellow students at the psychoanalytic institute were a provocative group—sardonic, sophisticated, and skeptical. Psychoanalysis has benefited from the Ph.D. crisis in the humanities; several of my most intellectually nimble colleagues would ordinarily have been on the tenure track. We were all older students, ranging in age from early thirties to early sixties. We did the assigned reading, and sometimes we would read aloud passages that we found striking. Some concepts still resonate with me. (Our “shadow life,” for example, is the one we might have lived if we had chosen differently—and which we carry with us as a form of psychic double-entry bookkeeping.) I have accepted that much of my behavior is driven by unconscious motives, which has relieved me of the burden of believing that my mental constructs embody reality.
Analysts often continue working into their seventies and eighties; some of the elders shuffling through the clinics and dayrooms of my institute had studied with people who knew members of Freud’s inner circle. This sense of continuity gives heft and credibility to an enterprise that has sometimes been too responsive to intellectual fashion. Every new (or old) idea that the academy champions becomes the subject of earnest articles in the psychoanalytic journals: “Freud and Intersectionality”; “Psychoanalysis and the White Gaze”; and so forth. One understands the urge to be responsive to events at a time when most patients must be bringing politics into the treatment room. For me, though, analysis was most persuasive when it remained slightly aloof from current events. We should resist the impulse to pathologize the views of those with whom we disagree.
The teaching at the institute was uneven, which was disappointing but not surprising. I’m sure I would have encountered the same problem in any graduate program, just as I had as a law student. What troubled me more was the gap I perceived between the knowledge claimed by the institute’s senior members about the origins and treatment of mental disorders and what seemed like an inability to answer basic questions. (For example, should we understand schizophrenia primarily as an organic brain disorder, or as a psychosocial problem?) More troubling still was their serene confidence in their treatment methods, despite the less-than-compelling scientific evidence for the effectiveness of those methods. To claim that psychoanalysis remains intact as a unified-field theory of mental disorders—to pretend, in other words, that it is 1957—will not do.
The neuropsychoanalysis movement “attempts to infuse into neuroscience some of the real, lived complexity of the life of the mind, and conversely, to introduce into psychoanalysis some of the scientific rigor of neuroscience,” in the words of Mark Solms, a South African psychiatrist and the acknowledged leader of the project. Solms, who trained for nine years at a London psychoanalytic institute and serves as the general editor of a new standard edition of Freud’s works, publishes prolifically in both neuroscientific and psychoanalytic journals. He and his colleagues aim to bridge the divide at the heart of modern psychiatry between biological and phenomenological—that is, narrative-based—approaches to understanding the mind. The late British neurologist Oliver Sacks wrote that the joining of neurology and psychoanalysis would be “a profound and almost unimaginable union . . . between the inner and outer approaches.”
Solms sees his work as “finishing the job that Freud began.” After all, Freud was a neuroscientist himself, one who accepted the existence of a natural science of the mind and who, in Solms’s view, abandoned biological methods “very reluctantly.” This attempt to buttress the reputation of analysis by reference to Freud’s own scientific grounding is not new. Of course, we know now that Freud was serially dishonest about his findings and methods, which tends to undermine his reputation as a scientist. With a few notable exceptions (the Nobelist Eric Kandel has said that psychoanalysis remains “the most coherent and intellectually satisfying view of the mind”), Freud’s reputation among neurologists and biologists is basically that of a vigorous charlatan.
Solms is brilliant and a charismatic evangelist. I wonder, though, whether neuropsychoanalysis is likely to be the savior that some analysts seem to hope, restoring Freud at last to a position of honor. I doubt that the best strategic path for analysis is to align itself with the biological approach. Analysis cannot ignore biology, but the biology of the mind is not the mind tout court. Neuroscientific research can tell us what areas of the mind are activated by dreaming, but it cannot tell us anything about the subjective experience of the dreamer or place her dream in the context of her personal history. For this, we need a patient and a clinician, and it is this encounter, for all its strangeness and subjectivity, that will be the source of psychoanalysis’s ongoing claim on our attention, if it has one.
Andrew Solomon, 59, is a lecturer in psychology at Columbia University and the author of several award-winning books, including The Noonday Demon: An Atlas of Depression (2001). In 1995, he was himself suicidally depressed. He was referred to an eminent psychoanalyst, Richard Friedman. Their relationship would last for 25 years, ending only with Friedman’s death in 2020. Of course, a decades-long consultation sounds like the setup to a Woody Allen punch line about analysis: “I think we may be starting to make progress.” But the extended reminiscence that Solomon published after Friedman’s death, “Obituary for the Analyst,” also reminds us of how complex, mysterious, and even beautiful the therapeutic process can be.
Solomon’s account largely contravenes common negative biases about analytic treatment. Analysis is often thought of as self-indulgent. We assume that patients want to be told that their suffering is the consequence not of their own choices but of their family dynamics or middle-class hypocrisy or political oppression. The reflexive conservative criticism of psychoanalysis and, more broadly, of the entire edifice of modern psychiatry is that it denies patients agency and thereby engenders learned helplessness.
Agency is precisely what Friedman tried to return to Solomon, who was burdened by self-defeating assumptions about what his life was going to be. Friedman told Solomon that he was not fated to have exploitative romantic relationships, as Solomon believed; that he was not weak, but strong; that he could make better choices. Crucially, Friedman did this without being gratifying or supportive or nonjudgmental in a conventional sense. As Solomon writes, he was sometimes rather severe:
Unlike my previous analyst, Dr. F was never seductive. . . . I wanted him to like me; I wanted everyone to like me. Yet even in the throes of my transference, I knew in those early days that his liking me was of little interest to him. . . . I couldn’t pretend that he romanticized or overestimated me, because he withheld reassurance about so many things on so many occasions.
This is what analysis should look like. One might object that “Dr. F” was a particularly gifted practitioner and that a method of treatment that requires genius is likely to be of little practical use. And, of course, Solomon was a perfect patient: from a wealthy family, intellectually gifted, and high in openness. Analysis has been defined as a process by which the patient becomes his own therapist—but for this, you need someone capable of insight. An analyst could spend an entire career chasing the kind of experience Solomon and his doctor shared. It must have been as gratifying to Dr. F as it was to his patient.
Through a combination of dubious doctrine and institutional arrogance, psychoanalysis earned its current position of exile from the American psychiatric mainstream. It will have to earn its way back, and in that effort, it will have many enemies, who would like to see it go the way of mesmerism and lobotomy. Among those enemies, the most powerful might be the health-insurance companies, which see in psychoanalysis a combination of grand claims, uncertain efficacy, and open-ended financial commitment. Mental-health parity legislation will make it easier for people seeking psychotherapy to get their sessions paid for by insurance, but whether their coverage will include extended psychoanalysis, or whether the insurers’ preference for medication and targeted therapies like CBT will prevail, is not clear. It may be that psychoanalysis will continue just as it is now, training a small number of dedicated adherents and relying on patients with a strong drive for psychic exploration and the means to pay for it.
Even the continued institutional decline of psychoanalysis won’t mean the disappearance of Freud as an intellectual totem. Many of his ideas now belong to a general inheritance. We may think of Freud as broadly debunked, like Ptolemaic cosmology, but we are all, to some extent, Freudians. Freud didn’t invent the unconscious, but he gave it the vocabulary that we use today. When we accuse our partners of being “defensive,” or ascribe a rival’s hostility to “projection,” we are speaking Freud, however imprecisely. Only the most rigid adherents to biological psychiatry would deny that psychotherapy has a place in the treatment of anxiety and depression. As America struggles to recover its equilibrium after a pandemic and amid ongoing political and economic turmoil, some of the people sitting in those wingback chairs, affirming their patients’ suffering, and aiming for Freud’s “evenly suspended attention,” will continue to be psychoanalysts.
In my experience, many young analysts are people of considerable intellectual ability, and most are strongly driven to meet their patients’ needs. They are unlikely to be classical Freudians, are more likely to be female or gay, and are less inclined than previous generations to claim the prerogatives of entitled professionals. They do not necessarily agonize over the truth of Freud’s core ideas. Young analysts generally assume that some of Freud is nonsense and that they’re capable of sorting wheat from chaff. They feel comfortable working with patients in whatever way seems most natural and effective. Most intend to integrate their analytic training with whatever predispositions they brought to it, whether formed in Ph.D. programs, in gay or feminist subculture, or in political activism. Such a diversity of approaches is, in some respects, healthy, but it also means that the field’s professional norms have weakened. There are now almost as many ways of working with patients as there are analysts. What was once a dogma is now merely an ethos.
Freud’s intellectual imperialism has not served psychoanalysis well. Not all the world’s problems, from the geopolitical to the interpersonal, can be solved by psychiatric intervention. Indeed, analysts must give themselves and their patients an honest account of how little we know about the sources and treatment of mental illness. The analyst who wants his patient to learn to tolerate ambiguity and doubt must start by learning to tolerate them himself, by recognizing that the patient’s dysphoria is not going to be solved by the “just so” stories of Freud’s case histories. It sometimes felt to me as though the analysts I spoke with knew both too little and too much.
What looks to outsiders like a crisis of psychoanalysis might not feel that way to those working in it. Many New York analysts continue to manage full practices, even if patients are no longer coming in the classically mandated three times a week. Younger analysts now completing their training and getting their licenses (in New York State, that of a licensed practitioner, or “L.P.”) are entering the field at a time when demand for outpatient mental-health services is extraordinarily high. Psychoanalysis is not intellectually respectable within mainstream psychology, but it has its own professional ecosystem and its own stars. Until recently, the field had been in steady decline for decades, but when I noted this situation, several analysts told me, in effect: “I’m not sure what you mean. I’ve never been busier.”
I have asked several analysts what vision of human thriving psychoanalysis aims toward. I have mostly been met with puzzlement, as though they had never given the question much thought. Even accepting that the stance of the classical analyst is necessarily withholding—so that the patient’s vacuum-filling fantasies about the analyst will be clinically useful—it seems self-evident that the analyst himself must be guided internally by some system of values, however opaque. Psychoanalysis is focused on meaning, but as a local, rather than a universal, concern. In this respect, then, it does not really address the broader spiritual and communitarian crisis facing America.
And yet, any psychotherapy that helps us tolerate our inevitable suffering with more grace and resilience has value and can justify itself without the buttress of scientism. The distress of our fellow citizens is vast and worthy of all the compassion we can summon. In the end, it is the care and not the theory that heals.
I did not finish my psychoanalytic training. There were complicating factors—family obligations, never enough time—and the financial incentives all lay on the side of the law. Above all, though, I did not think that I could take the leap of faith required to commit myself fully to analysis, and I knew that anything less than a full commitment would not be enough. The patient needs to feel that the person sitting across from him is as invested in the fight as he is and that the difficult, sometimes humiliating, work of analytic treatment serves a purpose. (They keep that box of tissues on the side table for a reason.) Analysts, like clergy, must occasionally suffer crises—after which, faith either returns or it doesn’t. But a jaded mental-health professional is no good to anyone.
The Stoics have something to tell us—especially us Americans, for whom perfectibility is a secular religion. To run from suffering is, paradoxically, to make it more fearsome. I am sympathetic with the idea that we need to pull up our socks, toughen up, get out of our own heads. Ninety percent of the time, that is the advice we need.
It’s not the right counsel, though, for the suicidally depressed, for victims of sexual violence, for those who feel irredeemably alone. Whether such people need psychoanalysis or CBT or a microdose of psilocybin must remain—for now, at least—an open question. Despite its checkered history, and despite considerable personal ambivalence, I find myself rooting for psychoanalysis. In its classical tradition, in the Freud who asks us to come to terms with sorrow and finitude, I can make out an idea of human flourishing that is worth fighting for.
Top Photo: Despite the continued institutional decline of psychoanalysis, few would deny that psychotherapy still has some place in the treatment of anxiety and depression. (MICROGEN IMAGES/SCIENCE PHOTO LIBRARY/GETTY IMAGES)

